In a world where health and well-being take center stage, there are certain aspects of our bodies that we often shy away from discussing openly. Urinary and bowel incontinence are two such issues that, despite their prevalence, tend to be relegated to hushed conversations and unspoken concerns. The truth is, these conditions affect millions of individuals, transcending age, gender, and background, and they can have a profound impact on one's quality of life.
But here's the good news: there is a wide array of medical treatments available that can help individuals regain control and dignity over their lives.
Welcome to a comprehensive exploration of the world of bladder and bowel incontinence treatments. In this blog, we will delve into the different types of incontinence, demystify the range of treatment options at your disposal, and empower you with the knowledge to make informed decisions about your health.
We understand that seeking help for incontinence can be a sensitive and sometimes daunting process, which is why we aim to create a supportive and informative space where you can find answers to your questions, debunk myths, and discover solutions that fit your unique needs.
Whether you're someone personally affected by bladder leaks or a caregiver seeking guidance for a loved one, this blog is your compass in navigating the often complex landscape of medical treatments. Our commitment is to provide clarity, understanding, and a sense of empowerment as we embark on this journey together toward regaining control and living life to the fullest.
So, let's break the silence, dissolve the stigma, and embark on this enlightening exploration of medical treatments for urinary and bowel incontinence. Your path to renewed confidence and a better quality of life starts here.
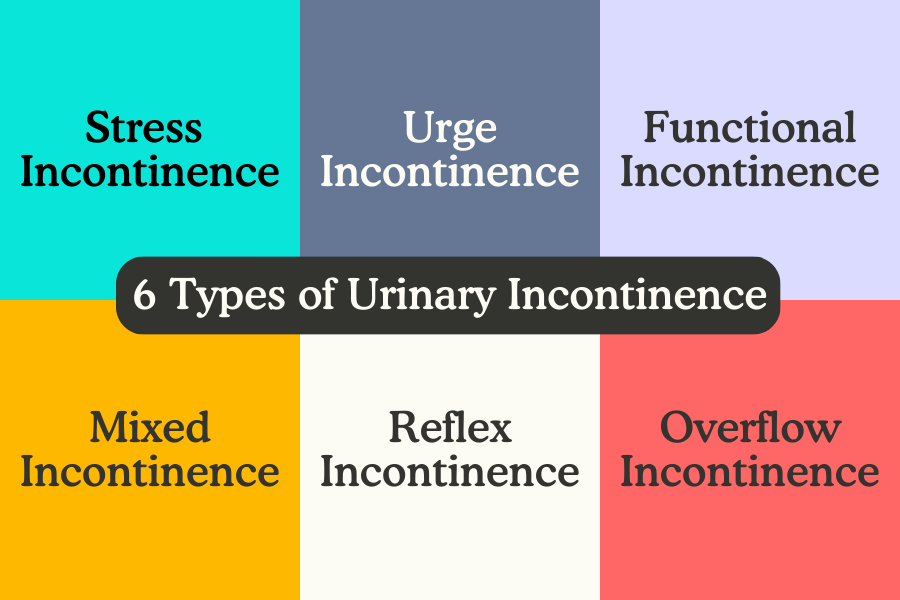
Understanding the Different Types of Incontinence
Before delving into the available treatment options, it's crucial to grasp the six distinct types of incontinence. Treatment plans for incontinence exhibit significant variability based on the specific type you might be encountering. Therefore, obtaining an official diagnosis is paramount, as it lays the foundation for tailoring an effective treatment strategy. There is no one cure for incontinence.
Stress Incontinence
Stress incontinence, a common subtype of urinary incontinence, manifests through a range of distinctive signs and symptoms. Individuals experiencing stress urinary incontinence often find themselves involuntarily leaking urine during activities that exert pressure on the bladder and pelvic region, such as coughing, sneezing, laughing, lifting heavy objects, or even minor physical movements. This condition is predominantly attributed to weakened pelvic floor muscles and inadequate support for the bladder and urethra.
Urge Incontinence, also known as Overactive Bladder or OAB
Urge incontinence, a form of overactive bladder, causes a sudden and intense urge to urinate, often with little to no warning. This urgent need to void is accompanied by an involuntary loss of urine, making it challenging to reach a restroom in time. People with urge urinary incontinence might find themselves frequently waking up at night to urinate (nocturia) or experiencing frequent bathroom trips during the day (increased frequency).
Functional Incontinence
This type of incontinence occurs when a person faces difficulties in reaching a restroom due to factors unrelated to the bladder or urinary system itself. Factors such as mobility issues, cognitive impairments, or environmental obstacles can contribute to functional urinary incontinence. Individuals experiencing this form of bladder leakage might exhibit signs of urgency, but the inability to navigate to a restroom in time leads to involuntary urine leakage.
Overflow Incontinence
Individuals with overflow incontinence often experience frequent or constant dribbling of urine, as the bladder becomes overfilled and unable to completely void. This can lead to a sense of incomplete emptying after urination, along with a weak or hesitant urinary stream. People affected by overflow urinary incontinence might find themselves making frequent trips to the restroom, yet only producing small amounts of urine. Additionally, they may have difficulty initiating urination and could experience straining. This condition is commonly associated with underlying medical conditions such as an enlarged prostate in men or neurological disorders that impact bladder function.
Reflex Incontinence
Reflex Incontinence is characterized by the release of urine with no warning or urge. Typically, reflex incontinence is due to nerve damage to the nerves responsible for signaling bladder fullness or emptiness. The most common appearance of this form of urinary incontinence is in people with severe brain damage or spinal cord injury, those with multiple sclerosis (MS), or those who have undergone radiation treatments or specific surgeries.
Mixed Incontinence
Individuals with mixed urinary incontinence often face a combination of involuntary urine leakage during activities that exert pressure on the bladder (stress incontinence) and sudden, intense urges to urinate followed by leakage (urge incontinence). This overlap of symptoms can lead to a significant impact on daily life, as individuals grapple with both physical and emotional challenges. Recognizing the coexistence of stress and urge incontinence symptoms is essential for accurate diagnosis and the formulation of a comprehensive treatment strategy tailored to addressing the complexities of mixed incontinence.
Fecal Incontinence
Bowel incontinence, also known as fecal incontinence, refers to an inability to control the passage of stool, leading to unexpected and involuntary leakage. This leakage can vary in severity, from small amounts of liquid stool to complete loss of bowel control. Those affected may experience an urgent need to empty the bowels or a feeling of incomplete evacuation even after a bowel movement.

Medications to Control Urinary Incontinence
Incontinence Drugs: How Do They Work?
For those navigating the challenges of urinary and bowel incontinence, finding effective solutions is paramount to restoring a sense of normalcy and quality of life. Incontinence drugs offer a diverse array of medications designed to target the underlying causes of various incontinence types, providing relief from symptoms and aiding in regaining control over bladder and bowel function.
From anticholinergics and beta-3 adrenergic agonists to topical treatments, this exploration of bladder incontinence medicine will shed light on how these medications work, their potential benefits, and the considerations involved in choosing the most suitable treatment for each individual's unique situation. It’s important to remember that while there is no one “cure” for bladder leakage there are prescriptions and treatments available that, when tailored to your specific set of symptoms, can help immensely with bladder control, urinary urgency, and urine leakage.
Anticholinergic Drugs
Anticholinergic drugs represent a class of prescriptions commonly prescribed for managing certain types of bladder incontinence, particularly overactive bladder (OAB) and urge incontinence. These prescription bladder control medications work by blocking the action of acetylcholine, a neurotransmitter that contributes to bladder muscle contractions and urgency sensations. By doing so, anticholinergic drugs help relax the bladder muscle, reduce involuntary contractions, and increase the bladder's capacity to hold urine, ultimately diminishing the frequency of urgent urges and episodes of leakage.
While offering relief from incontinence symptoms, it's important to note that anticholinergic drugs may also come with potential side effects, such as dry mouth, constipation, and blurred vision, which vary among different individuals and medications.
Beta-3 Agonists
Beta-3 agonists represent a newer class of prescription bladder control medications that have shown promise in treating overactive bladder (OAB) and urge incontinence. These incontinence drugs target the beta-3 adrenergic receptors found in the bladder's smooth muscle cells. By activating these receptors, beta-3 agonists promote relaxation of the bladder muscle, increase its capacity to hold urine and decrease the frequency and intensity of involuntary contractions that lead to urgency and leakage. What sets beta-3 agonists apart is their more selective action on the bladder muscles compared to other beta receptor types found in the heart and lungs, potentially reducing side effects often associated with other medications.

Hormonal Therapy for Bladder Control
Hormonal therapy for bladder control has emerged as a unique avenue for addressing certain types of urinary incontinence in women, particularly those associated with changes in estrogen levels due to factors such as menopause or hormonal fluctuations. Estrogen plays a pivotal role in maintaining the health and function of the pelvic floor muscles and tissues, which are crucial for bladder control. Hormonal treatments, often delivered through topical creams, vaginal rings, or tablets, aim to restore optimal estrogen levels in the vaginal and urethral tissues. By doing so, these treatments can enhance the integrity of the pelvic muscles and improve the overall tone and support of the bladder and surrounding structures.
Alpha-Blockers
Alpha-blockers, commonly prescribed for conditions like hypertension and benign prostatic hyperplasia (BPH), have also found application in managing urinary incontinence, particularly in cases related to overflow incontinence or functional obstruction of the bladder. These medications work by relaxing the smooth muscles around the urethra and bladder neck, facilitating easier urine flow and reducing resistance during voiding. For individuals with conditions like BPH or neurological disorders affecting bladder function, alpha-blockers can help alleviate symptoms such as hesitancy, weak urinary stream, and incomplete bladder emptying, which can contribute to overflow incontinence. While alpha-blockers can be beneficial for specific cases, their use should be closely monitored and tailored to the individual's needs, as they may be associated with side effects like dizziness, low blood pressure, and interactions with other medications.
Combination Medications
Combination therapy involving multiple medications has emerged as a strategic approach to address complex cases of urinary and bowel incontinence. This tailored medical treatment method involves prescribing different types of medications that target various aspects of incontinence, often working synergistically to provide comprehensive symptom relief. For instance, combining an anticholinergic drug with a beta-3 agonist can provide enhanced control over bladder contractions and urgency sensations.
Similarly, a multi-pronged approach might involve combining medications that address both the muscle-related aspects of incontinence and the underlying hormonal factors contributing to the condition. While combining medications can lead to improved efficacy, it's important to acknowledge potential interactions, side effects, and individual patient considerations. Healthcare professionals play a crucial role in evaluating the patient's medical history, symptoms, and goals to devise a combination therapy regimen that maximizes benefits while minimizing risks.
Interventional Therapies for Urinary Incontinence
While traditional approaches like medications and physical therapies remain integral, interventional therapies offer minimally invasive yet highly effective alternatives for individuals whose symptoms are not adequately controlled by conventional methods. We aim to empower individuals with the knowledge and understanding necessary to make informed decisions about their care and embark on a journey toward regaining control, comfort, and improved quality of life.

Sacral Neuromodulation (SNS)
Sacral Neuromodulation (SNS), also known as sacral nerve stimulation, is an advanced and innovative treatment option for individuals struggling with urinary and bowel incontinence, as well as related conditions like overactive bladder and fecal urgency. SNS involves the implantation of a small device, akin to a pacemaker, which delivers gentle electrical impulses to the sacral nerves responsible for regulating bladder and bowel function. These impulses help modulate nerve activity, effectively influencing pelvic floor muscles and the communication between the brain and the bladder or bowel. SNS is often considered when other treatments have proven ineffective or when patients are seeking long-term relief without the side effects associated with medications.
While SNS has shown remarkable success in improving symptoms and quality of life for many individuals, the procedure requires careful evaluation, as well as a trial period to ensure its effectiveness before permanent implantation.

Posterior Tibial Nerve Stimulation (PTNS)
Posterior Tibial Nerve Stimulation (PTNS) is an innovative and non-invasive treatment approach that offers relief to individuals grappling with urinary and bowel incontinence, as well as other pelvic floor disorders. During PTNS, a healthcare professional inserts a thin needle electrode near the ankle, which is then connected to a small device that delivers electrical impulses to stimulate the posterior tibial nerve. This nerve is linked to the sacral nerves, which play a crucial role in controlling bladder and bowel function. Through gentle and controlled stimulation, PTNS aims to modulate nerve activity, enhance pelvic muscle function, and improve communication between the brain and the bladder or bowel. This therapy for bladder control is typically administered in a series of sessions, providing a viable option for those seeking a minimally invasive alternative to medication or surgery.
With its impressive efficacy and relatively low risk of adverse effects, PTNS has become a valuable addition to the spectrum of treatments available for individuals striving to regain control over their urinary and bowel functions.

Botox Injections
Botox (botulinum toxin), commonly known for its cosmetic applications, has proven to be a transformative treatment option for certain types of urinary incontinence, particularly in cases of overactive bladder (OAB) that are unresponsive to other therapies. In this innovative approach, Botox is injected directly into the bladder wall or the muscle during a minimally invasive procedure. Botox works by temporarily paralyzing the muscles responsible for excessive contractions and urgency sensations. By doing so, it effectively reduces the frequency of involuntary bladder contractions and offers substantial relief from the symptoms of OAB, such as frequent urination and urgent urges. Botox treatment for incontinence often provides several months of relief before re-treatment may be necessary.
Bulking Agents
Bulking agents, also sometimes referred to by its brand name Bulkamid, have emerged as a valuable option in the spectrum of treatments for urinary incontinence, particularly stress incontinence. This non-surgical approach involves injecting specialized materials, often in gel or particle form, into the tissues surrounding the urethra. The goal is to augment the bulk and provide additional support to the urethral sphincter, thereby enhancing its ability to prevent urine leakage during activities that exert pressure on the bladder. Bulking agents essentially reinforce the structural integrity of the tissues, providing a mechanical barrier that reduces the chances of involuntary urine leakage. This procedure is minimally invasive and typically performed on an outpatient basis.

Surgical Treatments for Urinary Incontinence
For individuals facing persistent and severe urinary or bowel incontinence, surgical interventions offer a transformative path toward restoring control and enhancing their quality of life. While non-surgical approaches play a crucial role in managing these conditions, surgical treatments are often considered when other methods prove inadequate in providing relief.
Sling Procedures
Sling procedures represent a cornerstone of surgical treatments for urinary incontinence, specifically stress incontinence. These minimally invasive surgeries involve the placement of a supportive mesh sling under the urethra to provide enhanced structural support. By reinforcing the urethral sphincter and improving its ability to maintain continence during activities that exert pressure on the bladder, sling procedures effectively alleviate stress incontinence symptoms.
This approach is particularly beneficial for individuals whose incontinence is linked to weakened pelvic muscles or the weakening of the urethral support system. Sling procedures offer a high success rate, quicker recovery times compared to traditional open surgeries, and minimal scarring.
Bladder Neck Suspension
Bladder neck suspension, a surgical procedure commonly used to treat stress urinary incontinence, involves the repositioning and stabilization of the bladder neck, and urethra. This procedure is particularly beneficial for individuals whose leaky bladder is caused by a significant shift in the position of the bladder and urethra due to factors like childbirth or pelvic organ prolapse.
During the surgery, the bladder neck is lifted and secured to nearby pelvic ligaments or supportive structures, restoring its proper anatomical alignment and enhancing its ability to maintain continence during activities that trigger stress incontinence. Bladder neck suspension procedures have proven to be effective in providing long-term relief from stress incontinence symptoms.
Artificial Urinary Sphincter
Artificial urinary sphincters represent a sophisticated solution for individuals dealing with severe urinary incontinence, particularly when other treatments have proven ineffective. This surgical intervention involves implanting a device that mimics the natural function of the urinary sphincter—a muscular valve that controls urine flow. The artificial urinary sphincter consists of a cuff placed around the urethra, a pump implanted in the scrotum or labia, and a small reservoir implanted in the abdomen. By squeezing the pump, the cuff is inflated, closing off the urethra and preventing urine leakage. When the individual wishes to void, they can manually deflate the cuff using the pump, allowing urine to flow.
This technology offers a high degree of control over urinary function, enabling individuals to manage their incontinence effectively. However, artificial urinary sphincter surgery requires careful evaluation by a urologist or specialist, as it involves a more complex procedure and ongoing management to ensure optimal function and minimize complications.
Bladder Augmentation
Bladder augmentation, also known as cystoplasty, is a surgical procedure often considered for individuals with severe urinary incontinence or other bladder-related issues such as neurogenic bladder or interstitial cystitis. This complex intervention involves enlarging the bladder's capacity by grafting a segment of the individual's intestine onto the bladder wall.
By increasing the bladder's storage capacity, bladder augmentation aims to improve continence and alleviate symptoms associated with frequent urination, urgency, and leakage. While bladder augmentation can offer significant benefits, it's important to note that this procedure is typically reserved for cases where other treatments have failed and the impact on an individual's quality of life is substantial. Due to its complexity, potential risks, and long-term implications, a thorough evaluation by a urologist or specialist is essential to determine if bladder augmentation is a suitable option based on the individual's medical history, anatomy, and specific needs.
Colposuspension (Burch colposuspension)
Colposuspension is a surgical procedure designed to address stress urinary incontinence by providing support to the urethra and bladder neck. During this intervention, the surgeon lifts the front wall of the vagina and attaches it to the surrounding pelvic ligaments or tissue, effectively creating a hammock-like structure that lifts and stabilizes the bladder neck.
By restoring proper anatomical alignment, colposuspension enhances the urethral sphincter's ability to control urine flow during activities that trigger stress incontinence. This procedure has shown effectiveness in providing long-term relief from stress urinary incontinence symptoms.
Bladder Diversion Surgery
Bladder diversion surgery, also known as urinary diversion, is a complex procedure undertaken when individuals face irreversible bladder dysfunction due to factors like cancer, trauma, or congenital anomalies.
This surgical intervention involves rerouting the urinary tract to create an alternative way for urine to exit the body. There are various types of bladder diversion surgeries, including ileal conduit, continent urinary reservoir, and neobladder reconstruction.
In an ileal conduit, a section of the small intestine is used to create a stoma on the abdomen. From there, the ureters which carry urine from the kidneys to the bladder are attached to the other end of the intestine. Through this new pathway, the urine can be collected in the stoma and disposed of manually.
A Continent urinary diversion involves creating a reservoir inside the body to store urine, accessed periodically through a catheter. The ureters are attached to the pouch so the urine can flow freely. You can then insert a catheter through a stoma and manually release the urine.
Neobladder reconstruction aims to create a new bladder-like reservoir using a portion of the intestine.
While bladder diversion surgery offers individuals a way to manage their condition, it involves significant changes to daily routines and lifestyles.
Treatment Options for Fecal Incontinence
Bowel incontinence, a condition that affects individuals across different age groups, can be a source of significant physical and emotional distress. Fortunately, a range of treatments exists to address this challenging condition, offering hope and solutions for those seeking relief.
From non-invasive approaches like dietary modifications and pelvic floor exercises to more advanced interventions such as medications and surgical procedures, the landscape of treatments for faecal incontinence is diverse and evolving. This exploration delves into these various treatment options, shedding light on how they work, their potential benefits, and the considerations involved in selecting the most appropriate treatment path. By understanding these interventions, individuals can empower themselves to have informed discussions with healthcare professionals and embark on a journey toward regaining control, comfort, and improved quality of life.
Medications for Fecal Incontinence
Medications for bowel incontinence offer a viable avenue for a condition that can profoundly impact an individual's daily life. Depending on the underlying causes of bowel incontinence, different medications are prescribed to address specific aspects of the condition. Antidiarrheal medications, such as loperamide, aim to slow down bowel movements and reduce the frequency of urgency and accidents.
Fiber supplements can help regulate stool consistency and improve bowel regularity, potentially mitigating episodes of incontinence. Additionally, medications that target muscle contractions and sensitivity in the digestive tract, like antispasmodics, can contribute to better control over bowel movements.
While medications provide a non-invasive treatment option, their efficacy varies from person to person, and potential side effects must be considered.
Interventional Treatments for Bowel Incontinence
Interventional treatments offer a range of innovative approaches for managing bowel incontinence. Sacral nerve stimulation (SNS), for instance, involves the implantation of a device that delivers gentle electrical impulses to the nerves controlling bowel function, enhancing muscle control, and reducing incontinence episodes.
Biofeedback therapy utilizes sensors and visual feedback to train individuals to better control their pelvic muscles, improving muscle strength and coordination.
Injectable bulking agents can be used to reinforce the anal sphincter, helping to reduce leakage. While interventional treatments offer promising results, individual suitability varies, and consultation with a healthcare professional experienced in colorectal health is essential to determine the most appropriate treatment approach based on the individual's medical history and specific type of bowel incontinence.
Surgical Intervention for Bowel Incontinence
Surgical intervention serves as a vital option for individuals facing persistent and severe bowel incontinence that is resistant to other treatments. Surgical procedures aim to address the underlying causes of bowel incontinence, such as muscle dysfunction or structural abnormalities, to improve control over bowel movements.
Sphincteroplasty, for example, repairs damaged anal sphincter muscles to enhance their function and reduce leakage.
Artificial bowel sphincter implantation (ABS) involves placing a device that mimics the natural sphincter's role, providing better control over bowel movements.
In more complex cases, colostomy or ileostomy procedures reroute the bowel to create a stoma, allowing waste to exit the body through a pouch, effectively managing incontinence. While surgical interventions offer potential solutions, the decision to undergo surgery should be made in collaboration with a specialist in colorectal health.
If you are experiencing difficulties with urinary or fecal incontinence and have already attempted conservative measures such as bladder support supplements, pelvic floor physical therapy, and bladder protection products without achieving the desired results, it could be prudent to consult your healthcare provider regarding your subsequent actions.
Each diagnosis of incontinence is unique, underscoring the significance of thoroughly addressing all your symptoms and apprehensions with a qualified specialist. This approach will enable you to identify the most suitable incontinence treatment for your specific situation. It is essential to meticulously consider the advantages and disadvantages of each treatment approach!

Want to hear from others going through the same situation you are? Join our support groups!
Women’s Incontinence Support Group
Men’s Incontinence Support Group
Sources:
National Center for Biotechnology Information (NCBI). (2018). Urge incontinence. In StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK563172/#:~:text=Urge%20incontinence%20is%20a%20type,social%20stigma%20attached%20to%20it.
Cleveland Clinic. (n.d.). Functional incontinence. Retrieved from https://my.clevelandclinic.org/health/diseases/24858-functional-incontinence
Cleveland Clinic. (n.d.). Acetylcholine (ACh). Retrieved from https://my.clevelandclinic.org/health/articles/24568-acetylcholine-ach#:~:text=Acetylcholine%20(ACh)%20is%20a%20neurotransmitter,%E2%80%9Cfire%20off%20the%20message.%E2%80%9D
Urology Times. (2018). Beta-3 agonists: A much-needed alternative for patients with OAB. Retrieved from https://www.urologytimes.com/view/beta-3-agonists-a-much-needed-alternative-for-patients-with-oab
UpToDate. (n.d.). Urinary incontinence treatments for women (Beyond the Basics). Retrieved from https://www.uptodate.com/contents/urinary-incontinence-treatments-for-women-beyond-the-basics#:~:text=Topical%20vaginal%20estrogen%20%E2%80%94%20Vaginal%20estrogen,and%20vaginal%20atrophy%20(dryness).
National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). (n.d.). Prostate enlargement (benign prostatic hyperplasia). Retrieved from https://www.niddk.nih.gov/health-information/urologic-diseases/prostate-problems/prostate-enlargement-benign-prostatic-hyperplasia#:~:text=Benign%20prostatic%20hyperplasia%E2%80%94also%20called,periods%20as%20a%20man%20ages.
Kaiser Permanente. (n.d.). Urethral sling surgery. Retrieved from https://healthy.kaiserpermanente.org/health-wellness/health-encyclopedia/he.urethral-sling-surgery.hw219880
Mercy Health. (n.d.). Surgical bladder suspension. Retrieved from https://www.mercy.com/health-care-services/urology/treatments/surgical-bladder-suspension
MedlinePlus. (n.d.). Bladder outlet obstruction (BOO). Retrieved from https://medlineplus.gov/ency/article/003983.htm
Cleveland Clinic. (n.d.). Augmentation cystoplasty (bladder augmentation). Retrieved from https://my.clevelandclinic.org/health/treatments/15846-augmentation-cystoplasty-bladder-augmentation
Your Pelvic Floor. (n.d.). Colposuspension for stress incontinence. Retrieved from https://www.yourpelvicfloor.org/conditions/colposuspension-for-stress-incontinence/#:~:text=to%20this%20operation%3F-,What%20is%20colposuspension%3F,ligaments%20to%20elevate%20the%20vagina.
Bladder Cancer Advocacy Network (BCAN). (n.d.). What is an ileal conduit? Retrieved from https://bcan.org/what-is-an-ileal-conduit/
National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). (n.d.). Urinary diversion. Retrieved from https://www.niddk.nih.gov/health-information/urologic-diseases/urinary-diversion#:~:text=Continent%20urinary%20diversion%20allows%20you,is%20placed%20inside%20your%20abdomen.
Mayo Clinic. (n.d.). Neobladder reconstruction. Retrieved from https://www.mayoclinic.org/tests-procedures/neobladder-reconstruction/about/pac-20385066#:~:text=Neobladder%20reconstruction%20is%20a%20surgical,one%20option%20for%20urinary%20diversion.
Harvard Health Blog. (2019). Treating constipation with biofeedback for the pelvic floor. Retrieved from https://www.health.harvard.edu/blog/treating-constipation-with-biofeedback-for-the-pelvic-floor-2019051616638
Baylor College of Medicine. (n.d.). Anal sphincteroplasty. Retrieved from https://www.bcm.edu/healthcare/specialties/obstetrics-and-gynecology/urogynecology/procedures/anal-sphincteroplasty#:~:text=Content,muscles%20that%20control%20bowel%20movements.
Galliano Surgery. (n.d.). Artificial bowel sphincter (ABS). Retrieved from https://www.gallianosurgery.com/ABS.shtml#:~:text=Procedure%20for%20ABS&text=It%20must%20be%20inserted%20by,the%20balloon%20to%20the%20cuff.









